Contextualized Veterinary Care: Matching medicine to context (#389)
- Rick LeCouteur
- Aug 11, 2025
- 4 min read
For decades, small-animal practice often equated gold standard with the most technologically intensive, and expensive, path.
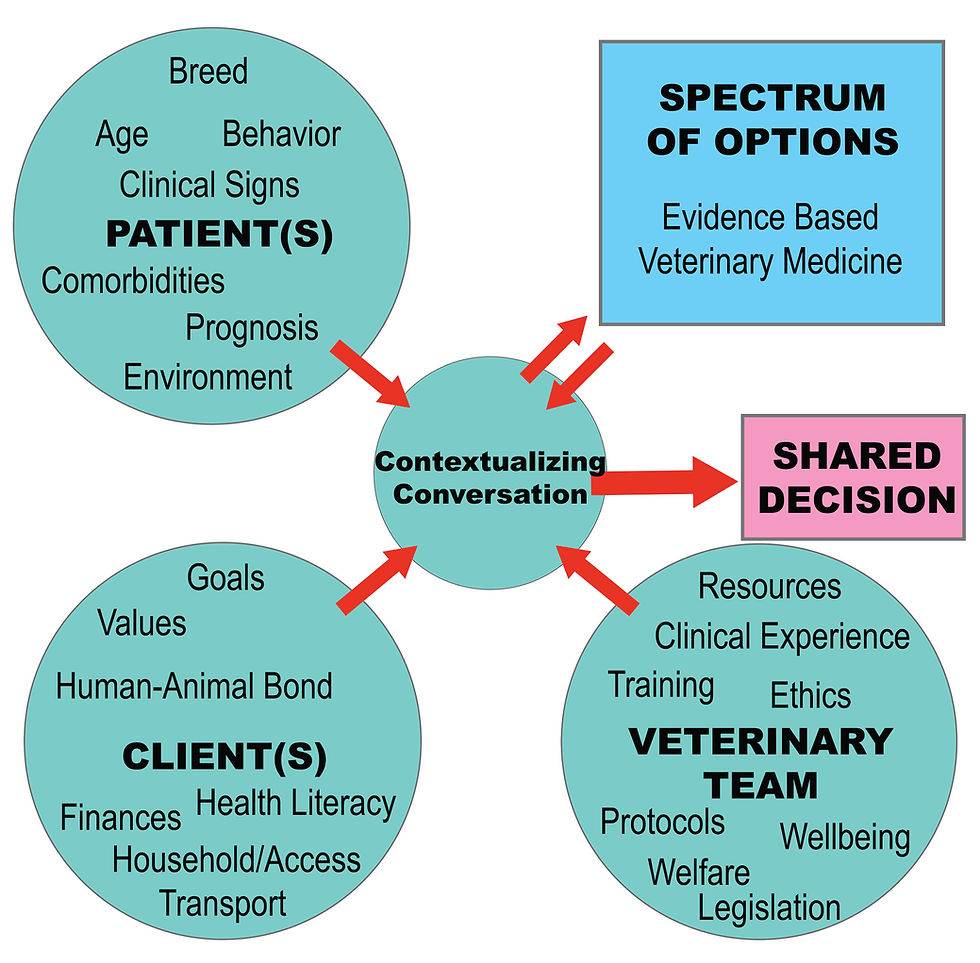
That mindset is shifting. Veterinary teams are increasingly embracing Contextualized Care (also called Spectrum of Care), which grounds medical decisions in the best available evidence and the lived realities of each client, patient, and practice.
At the center of this model is communication.
Clients, for their part, want a clear picture: a range of options, what each entails for their animal, pros and cons, and costs. When invited into that process, most prefer a collaborative approach to decisions. This is the heart of shared decision-making.
What Does Contextualized Actually Mean?
Contextualized care doesn’t mean lowering standards; it means matching care to context, including the patient’s needs, the client’s goals and constraints, and the team’s resources, while staying anchored in evidence-based veterinary medicine.
Shared Decision-Making: Three Talks, One Decision
Elwyn et al.’s three-talk model offers a simple, repeatable scaffold for shared decision-making in everyday practice:
Team talk – Level the power dynamic. Invite the client—and when helpful, family members or other team members—into the process and set shared goals.
Option talk – Lay out each option’s advantages, disadvantages, and costs, while pausing to ensure understanding and encourage questions.
Decision talk – Deliberate back-and-forth to surface the client’s informed preferences and arrive at a plan that fits the patient and situation.
This structure reliably supports contextualization across preventive, problem, and urgent-care visits.
The Communication Toolbox (What To Do In the Room)
Coe et al. offer a compact toolbox any clinician can deploy without any extra equipment: introductions, open-ended inquiry, listening (including silence and reflective summaries), empathy (including “I wish…” statements), partnership language, summarizing, signposting, chunk-and-check, and presenting options.
Why these matter:
Open-ended inquiry (“Tell me…/Walk me through…”) elicits values, expectations, and constraints you’d otherwise miss.
Empathy & “I wish…” validate emotion and reduce conflict when hopes outpace what’s medically safe or feasible.
Partnership statements (“let’s…”, “together…”) mitigate perceived power imbalances.
Signposting & chunk-and-check give structure, support recall, and ensure informed consent is truly informed.
This humanistic style is especially important when serving diverse and historically marginalized communities; it creates a safe space for clients to share their realities without judgment.
Make Trade-offs Visible: The Value Matrix
Presenting options verbally can overwhelm. The Value Matrix turns the conversation into a co-created visual: list options down the left, context-specific pros/cons across the top, and fill cells with simple symbols (✔, ✖, ?). Then add comparable costs as a final column. Review columns (what matters most?) and rows (which option has the most ✔ with the fewest ✖ for this client/patient?).
In Coe et al.'s article, feline hyperthyroidism is used as an example. Two guardians with different capacities and concerns arrive, via shared decision-making and the Value Matrix, at different, both welfare-appropriate plans. The veterinarian reflects that stepping in with a single best answer would have missed what ultimately worked for each pair.
Why This Approach Improves Care
Practiced broadly and intentionally, contextualized care improves access and client adherence, because people feel heard and see options that genuinely fit their situation.
Plans can be revisited as contexts change, which is another key benefit.
Adopting contextualized care can also challenge identity for clinicians trained in a paternalistic “gold-standard-only” paradigm, and it may surface moral distress. Naming that, and offering support and training, helps teams move from a rigid one right answer stance to an evidence-based many right answers mindset that often reduces moral distress and burnout by restoring agency.
Professional regulators are increasingly publishing guidance that supports contextualized care, and shared decision-making satisfies the legal requirements for informed consent.
Five Things You Can Do Tomorrow
Open with roles and goals. “How would you like me to address you? What’s most important to you for Bella today?”
Elicit context early. Walk through the pet’s day, who’s involved in care, transport, budget, and home environment.
Frame options visually. Co-build a one-page Value Matrix and include comparable costs.
Use partnership language and “I wish…” when medicine and means collide.
Summarize and check. Close with a brief recap and a plain-language check for understanding.
Rick’s Commentary
Contextualized care doesn’t abandon excellence.
It redefines excellence as evidence-based care that fits.
With a simple shared decision-making structure and a handful of communication tools, any team can widen access, strengthen trust, and still honor the welfare of the patient.
That’s not a step down from the gold standard.
It's how we make high-quality veterinary medicine work in the real world.
Sources
Elwyn G, et al. A three-talk model for shared decision making: Multistage consultation process. https://www.bmj.com/content/359/bmj.j4891
Coe JB, et al. Clinical communication tools for contextualizing spectrum of care. https://www.advancesinsmallanimalcare.com/article/S2666-450X(25)00013-6/fulltext



Comments